Chronobiology and MSDs: What Kind of Causality?
Multiple factors influence the onset of musculoskeletal disorders (MSDs): biomechanical strains, organizational, environmental and psychosocial factors… but also individual factors that are sometimes less visible.
Among these, biological rhythms, and more broadly chronobiology, have attracted growing interest in recent years for understanding mechanisms of fatigue, recovery and vulnerability within the musculoskeletal system.
So, is there a causal link between disrupted biological rhythms and the emergence of MSDs? What mechanisms could explain it, and what are the current limits of scientific knowledge? Let’s take a closer look at this issue and at what science can (or cannot yet) assert on the matter!
Chronobiology: An Essential Reminder
Chronobiology, from the Greek chronos (time), refers to the study of biological rhythms within the body. In humans, the best known is the circadian rhythm : a cycle of about 24 hours that regulates numerous physiological functions, such as sleep, blood pressure, and body temperature.
In short, almost all biological functions are governed by this circadian rhythm, which is linked to our internal clock, located in the hypothalamus and influenced by light.
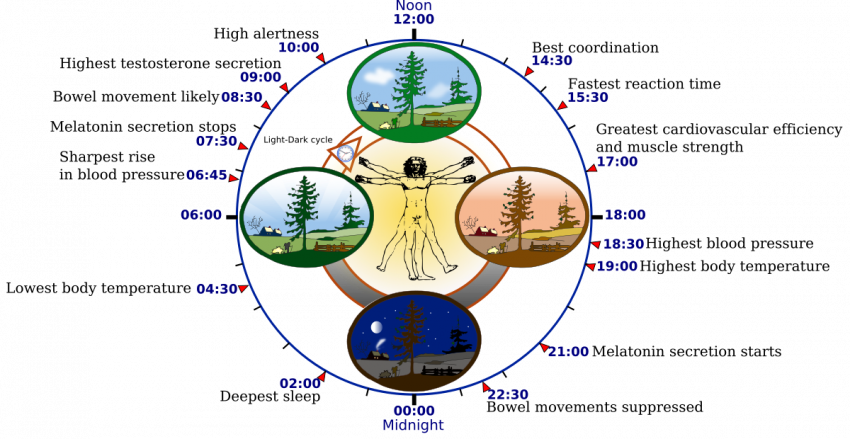
Credit : Wikipédia
MSDs: A Key Reminder
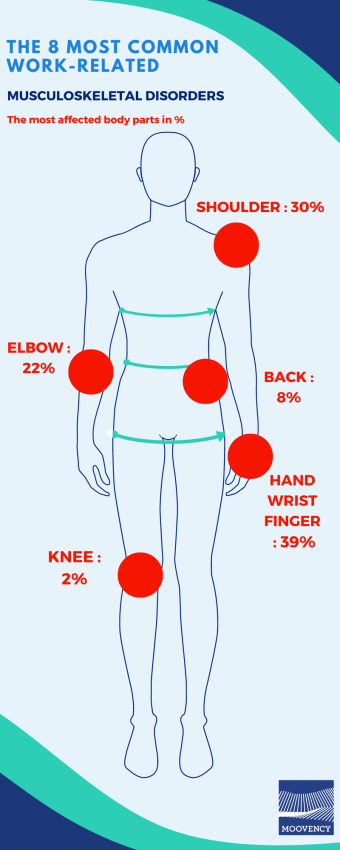
Musculoskeletal disorders (MSDs) are multifactorial conditions that encompass a wide range of impairments affecting joints, including muscles, tendons, nerves, and articulations. Their onset is often linked to repetitive activities, awkward postures, or prolonged physical effort.
These conditions represent a major challenge in occupational health: in 2024, MSDs accounted for nearly 90% of all occupational diseases in France.
A few key figures:
-
The leading cause of occupational illness in France and in many other countries.
-
Nearly 60% of women and more than 50% of men report pain related to back or upper-limb MSDs.
-
Worldwide, 494 million people suffered from other musculoskeletal disorders in 2020—an increase of 123.4% in the total number of cases compared with the 221 million recorded in 1990.
What Is the Impact of Chronobiology on the Onset of MSDs?
Even though current research remains limited, several physiological mechanisms can help explain how a disruption in biological rhythms might contribute to the emergence or worsening of musculoskeletal disorders (MSDs).
To date, no study has demonstrated a direct causal link between circadian disruptions and MSDs. However, several physiological mechanisms suggest possible, but not decisive, amplifying pathways.
First Indirect Pathway → Circadian Rhythms and Muscle Recovery
Muscles, tendons, bones, and cartilage all possess their own biological clocks, responsible for synchronizing repair and regeneration cycles:
→ muscle strength varies depending on the time of day (performance peaks)
→ tissue repair capacities follow cyclical patterns
→ collagen production and tendon regeneration are more effective at night
When the circadian rhythm is disrupted, muscle recovery becomes less efficient, which can increase micro-injuries, pain, and overall sensitivity to movement and exertion.
Second Indirect Pathway → Poor Sleep = Impaired Tissue Repair
Sleep, a cornerstone of chronobiology, plays a key role in pain modulation, nervous system regulation, and muscle recovery.
Sleep disturbances or day–night disruption reduce the secretion of hormones essential for muscle restoration (e.g., growth hormone), leading to poorer tissue repair and increased inflammation.
Altered sleep thus becomes an aggravating factor that can intensify pain perception and diminish muscular recovery, ultimately increasing vulnerability to MSDs.
Third Indirect Pathway → Cognitive Fatigue and Posture
Circadian misalignment impacts:
→ alertness
→ motor precision
→ muscle tone
→ concentration
In the workplace, this may translate into inadequate postures, less precise movements, compensatory postures, and faster onset of fatigue. These behaviors increase the actual mechanical load on tissues and therefore the risk of MSDs in repetitive tasks or activities requiring sustained posture.
Key Takeaway
DISRUPTION OF THE CIRCADIAN RHYTHM
↓
Degraded sleep + reduced muscle recovery + fatigue + inflammation
↓
Potentially increased vulnerability to MSDs
The Case of Workers with a Shifted Circadian Rhythm
The mechanisms described earlier become particularly relevant when looking at populations whose circadian rhythm is regularly desynchronized. This is especially true for night workers, evening workers, rotating-shift workers, rapid-rotation workers, or anyone exposed to irregular schedule variations.
Night work or rotating shifts expose the body to a partial or complete inversion of the day–night cycle. This leads to reduced sleep quality, irregular recovery cycles, and hormonal disruption (melatonin, cortisol).
These chronic disturbances create a context that increases the likelihood of faster fatigue, reduced alertness at the end of a shift, and greater motor compensations. One can therefore assume an amplified vulnerability that adds to the physical demands already present in these occupations.
To Conclude…
Circadian desynchronization weakens several essential mechanisms: sleep quality, muscle recovery, hormonal regulation, alertness, and motor precision. However, chronobiology is not currently considered a direct, established risk factor for MSDs.
Its inclusion in risk assessment can therefore be beneficial, provided that its impact is not overestimated in relation to other key risk factors.
A Few Recommendations…
-
Act on work schedules: encourage regular shifts and limit overly frequent changes. Favor forward-rotating schedules (morning → afternoon → night).
-
Optimize night work: regular breaks, rest areas, and increased alertness during circadian low points.
-
Strengthen recovery: by stabilizing lifestyle habits as much as possible (sleep, diet, physical activity).
-
Adjust physical load by accounting for chronobiological factors: reduce loads or optimize tools during periods when muscular capacity is physiologically lower.
-
Improve consideration of psychosocial factors: circadian disruption heightens sensitivity to stress—enhance managerial support, autonomy, and schedule predictability.
-
Train teams: prevention principles, ergonomic gestures and postures. Emphasize that primary prevention remains the priority, but rhythm management is a complementary lever.
Discover our related articles on the topic
Sources :
Ameli – Understanding musculoskeletal disorders
Apivia – Chronobiology : https://www.apivia.fr/actualites/toute-l-actu/la-chronobiologie/
Gill, Tiffany K et al. – Global, regional, and national burden of other musculoskeletal disorders, 1990–2020, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021
https://www.thelancet.com/journals/lanrhe/article/PIIS2665-9913(23)00232-1/fulltext
Juliana N, Azmi L, Effendy NM, Mohd Fahmi Teng NI, Abu IF, Abu Bakar NN, Azmani S, Yazit NAA, Kadiman S, Das S. – Effect of Circadian Rhythm Disturbance on the Human Musculoskeletal System and the Importance of Nutritional Strategies
https://pmc.ncbi.nlm.nih.gov/articles/PMC9920183/#sec3-nutrients-15-00734



